Cardiovascular Disease, Mood Disturbance, and Cognitive Deficits
by London Butterfield, Ph.D.
all rights reserved Clinical Psychology Associates of North Central Florida CPANCF.COM
2121 NW 40th Terrace Ste. B., Gainesville, FL 32605 352-336-2888
Cardiovascular disease (CVD), which comes in many forms and can affect people of all ages, refers to a variety of diseases that affect the cardiovascular system (i.e., heart,  blood vessels). Several types of CVD exist, including hypertension, coronary artery disease/atherosclerosis, cardiomyopathy, cardiac dysrhythmia, myocarditis, valvular heart disease, and heart failure. With low cardiac output resulting in reduced cerebral perfusion, patients with CVD are at greater risk for cerebrovascular disease and for cognitive deficits, including problems with memory, attention, psychomotor speed, and executive functioning. Eggermont et. al, (2014) found that lower cardiac output and worse left ventricular diastolic function were associated with executive function deficits. blood vessels). Several types of CVD exist, including hypertension, coronary artery disease/atherosclerosis, cardiomyopathy, cardiac dysrhythmia, myocarditis, valvular heart disease, and heart failure. With low cardiac output resulting in reduced cerebral perfusion, patients with CVD are at greater risk for cerebrovascular disease and for cognitive deficits, including problems with memory, attention, psychomotor speed, and executive functioning. Eggermont et. al, (2014) found that lower cardiac output and worse left ventricular diastolic function were associated with executive function deficits.
Research also shows that CVD is a risk factor for later severe cognitive impairment, including dementia (e.g., Alzheimer’s disease, cerebrovascular dementia).
Common co-morbid mood disorders, such as depression and anxiety, are frequently underdiagnosed and undertreated in patients with cardiovascular disease (CVD). Presence of common depressive symptoms such as sad or poor mood, decreased energy, feelings of agitation, feeling of guilt or worthlessness, loss of pleasure in activities, crying spells, concentration/attention problems, sleep and/or appetite disturbance, hopelessness, and thoughts of death has been associated with cognitive impairment and for the development of dementia. These are also considered a risk factor for the development of CVD and are associated with increased risk of death after an index myocardial infarction. Multiple episodes of depression, even including minor or subclinical depression, increases risk for dementia.
The relationship between CVD, depression, cognitive impairment and health care costs associated with poorly managed disease and complications highlights the importance of psychological diagnostic assessment and the monitoring of psychological and cognitive functioning in patients with CVD. Proper psychological assessment and treatment is also necessary because of the negative impact mood disorders and cognitive impairment can have on quality of life and well-being.
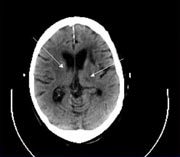 A comprehensive neuropsychological evaluation that assesses cognitive domains commonly affected in CVD as well as motor functions and psychological symptoms can help patient’s understand why they may be struggling with certain daily functions, shed light on a patient’s prognosis, and provide valuable recommendations for treatment. This may be particularly important for high functioning individuals who experience levels of deficits that may impact on their occupational functioning and responsibilities but which are far milder than those typically picked up on by neurological examinations or cognitive screening measures such as the Mini Mental Status Examination. A comprehensive neuropsychological evaluation that assesses cognitive domains commonly affected in CVD as well as motor functions and psychological symptoms can help patient’s understand why they may be struggling with certain daily functions, shed light on a patient’s prognosis, and provide valuable recommendations for treatment. This may be particularly important for high functioning individuals who experience levels of deficits that may impact on their occupational functioning and responsibilities but which are far milder than those typically picked up on by neurological examinations or cognitive screening measures such as the Mini Mental Status Examination.
Clinical and health psychologists provide interventions for general health and lifestyle issues that are, in many instances, problematic for individuals with CVD, including smoking cessation, stress management, and weight management. Psychologists can address mood disorders through psychotherapy and may offer cognitive rehabilitation with those who have cognitive deficits. Most psychologists use an eclectic therapeutic approach for treatment of mood disorder in cardiovascular patients (cognitive-behavioral, psychodynamic, insight-oriented, psychoeducational, and supportive). During cognitive rehabilitation, psychologists assist patients to learn strategies to improve their memory, attention, speed of processing, and executive functioning.
Importantly, with proper medical, psychological and neuropsychological care, cognitive effects of CVD are often reversible in certain patients if identified early enough. Early psychological interventions into health habits and making lifestyle changes can improve cardiac and cerebrovascular risk factors such as poorly controlled blood pressure, alcohol use, and exercise levels. However, restoration of cognitive deficits may be more difficult once morphological and functional changes have begun. Early identification of cardiovascular and cognitive problems should prompt patients and their health care providers to begin implementing effective interventions to help prevent further decline.
Further Readings:
Dardiotis E, Giamouzis G, Mastrogiannis D, Vogiatzi C, Skourlarigis J, Triposkiadis F, & Hadjigeorgiou GM (2012). Cognitive Impairment in Heart Failure. Cardiology Research and Practice, 2012 (2012), Article ID 595821, 9 pages.
de la Torre JC (2012). Cardiovascular risk factors promotor brain hypoperfusion leading to cognitive decline and dementia. Cardiovascular Psychiatry and Neurology, 2012 (2012), Article ID 367516, 15 pages.
Eggermont LHP, de Boer K, Muller M, et al Cardiac disease and cognitive impairment: a systematic review
Heart 2012;98:1334-1340.
Elias MF, Goodell AL, & Dore GA (2012). Hypertension and cognitive functioning: A perspective in historical context. Hypertension, 60, 260-268.
Vogels RLC, Scheltens P, Schroeder-Tanka HM, & Weinstein HC (2007). Cognitive impairment in heart failure: A systematic review of the literature. European Journal of Heart Failure, 9, 440-449.
Wint D (2011). Depression: A shared risk factor for cardiovascular and Alzheimer disease. Cleveland Clinic Journal of Medicine, 78 (Supplement 1), S44-S46.
Published: 1/2/12 updated with new edits 7/22/23
Editor: Ernest J. Bordini, Ph.D. Licensed Psychologist
Clinical Psychology Associates of North Central Florida offers a range of clinical and health psychology services including psychological and neuropsychological assessment, behavioral medicine assessments, pre-surgical assessment, and psychotherapy services. Appointments can be scheduled by calling (352) 336-2888
CPANCF does not endorse or make any warranties about the below advertising:
|

