| |
Autism Spectrum Disorder DSM –5 Diagnosis
Clinical Psychology Associates of North Central Florida, more than 30-years of experience in the comprehensive pediatric neuropsychological assessment of Autism Spectrum and Related Disorders. This page provides information about the history of diagnosing Autism Spectrum Disorders (ASD), approaches in assessing the complexities of the disorder, and links to more information, evidence-based treatment approaches, and resources for children, adolescents and Adults with ASD.
We offer in-person assessments in our offices in Gainesville and Ocala FL (352)-336-2888
What are Autism Spectrum Disorders?
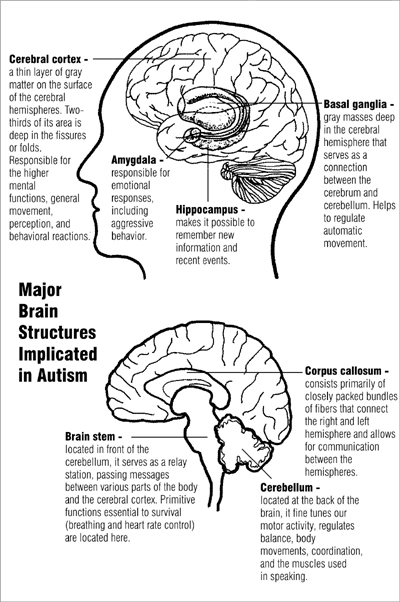
Autism Spectrum Disorders are significant and complex neurodevelopmental disorders impacting on reciprocal relationships which are usually evident and diagnosed by early childhood or adolescence. Difficulties in practical verbal and nonverbal social communication, repetitive or stereotyped interests and mannerisms are common manifestations of the disorders. Delays in developmental milestones, especially for communication are often evident. For a discussion of the origins of the diagnosis of autism, theories about causes of Autism Disorders, and DSM-IV criteria and assessment see this article from our neuropsycholgycentral.com website: Autism Etiology and Assessment.
A list of common signs of Autism Spectrum Disorder in toddlers, preschoolers, children, adolescents, and young adults can be found on signs and symptoms page at AutismSpectrumAsssment.com website.
How are Autism Spectrum Disorders Diagnosed?
 DSM-5, the Diagnostic and Statistical Manual published by the American Psychiatric Association was adopted in 2013. One of the major changes has been how it classifies a group of disorders which usually manifest in childhood and adolescence. Autism Spectrum Disorder now encompasses former DSM-IV distinct categories of “classic” Autism, Asperger’s Disorder, a rather loosely formulated disorder referred to as Pervasive Development Disorder (PDD), and Childhood Disintegrative Disorder. DSM-5, the Diagnostic and Statistical Manual published by the American Psychiatric Association was adopted in 2013. One of the major changes has been how it classifies a group of disorders which usually manifest in childhood and adolescence. Autism Spectrum Disorder now encompasses former DSM-IV distinct categories of “classic” Autism, Asperger’s Disorder, a rather loosely formulated disorder referred to as Pervasive Development Disorder (PDD), and Childhood Disintegrative Disorder.
Some major changes in exclusionary criterion involve removal of much of the references to language delays or disorders. DSM-5 incorporates emerging research and conceptual trends which view these childhood disorders as a range, or spectrum of disorders, of varying severity. The more specific criteria most likely will exclude some children previously diagnosed in the rather loosely-defined diagnosis of Pervasive Developmental Disorder and it may have further benefit of preventing some children with Attention-deficit Hyperactivity Disorder, who typically have milder social skill deficits from being misdiagnosed or “over-diagnosed” as suffering an Autism Spectrum Disorder.
While most children with Autism Spectrum Disorder show early characteristic problems with eye contact, stereotypic or repetitive motor behaviors and interests, and rather marked difficulties in interactive play and other symptoms at an early age, DSM-5 reflected increased recognition that for some children, the deficits in reciprocal social interaction may not manifest until expectations for social roles, demands and interactions exceed limited capacities, and thus might be diagnosed later. The DSM-5 emphasis on the limitation and impairment of everyday activities also suggests emphasis on a more empirical assessment of adaptive behavior.
To meet diagnostic criteria for ASD under DSM-5 all common symptom clusters must be met for Autism Spectrum Disorder. This includes persistent deficits and social interaction across contexts including 1) deficits in social-emotional reciprocity. 2. Deficits in nonverbal communicative behaviors; and 3. Deficits in developing and maintaining relationships. Children must demonstrate restricted and repetitive patterns of behavior, interests or activities. Symptoms must be present in early childhood. Symptoms must also together limit and impair everyday activity.
Are Autism Spectrum Disorders being diagnosed more frequently?
There have been debates about the reasons for increased diagnosis of Autism Spectrum Disorder over time, and the DSM-5 adopted in 2013 moved to incorporate some looser categories into a diagnostic conceptualization with more specific criteria and a continuum in terns of range of severity. The CDC’s Autism and Developmental Disabilities Monitoring (ADDM) Network notes that even with the revised criteria, there was an increase from 1 in 150 children in 2000 to 1 in 36 children in 2020. While there is little consistent evidence of differences in rates for race or ethnicity, ASD is nearly 4 times more common among boys than among girls.
What are the Complexities of Autism Spectrum Disorder and Differential Diagnosis?
The complexity of differential diagnosis is further complicated by the fact these disorder can be co-morbid. Research cited on Autism.org notes that almost 40% of children with autism and 50% of adults with autism have a variety of comorbid anxiety disorders. Hudson, et., al (2019) conducted a meta-analysis and found that the pooled lifetime prevalence of depressive disorders in individuals with ASD was 14.4% (95% CI 10.3–19.8). AutismSpeaks.org estimates depression affects an estimated 7% of children and 26% of adults with autism.
Another development in DSM-5, relevant to the diagnostic differential of Autism Spectrum Disorder, is the introduction of Pragmatic Social Communication Disorder (SCD)as a diagnosis. SCD often presents with impairments in verbal and nonverbal communication, language processing, social cognition, and pragmatics. While a relatively new diagnosis, Ketelaars et. al. (2009) suggested that pragmatic language impairments can affect up to 7.5% of children and may be twice as prevalent in males than females.
While children and adults with Autism or Pragmatic Social Communication Disorder (SCD) all have difficulties with social communication, a diagnosis of ASD also requires repetitive and/or disruptive behaviors. In such cases, the presence of restricted/repetitive patterns of behavior, interests, or activities in individuals with autism and their absence in social (pragmatic) communication disorder helps differentiate between the disorders. Children with ASD may perform poorly on social pragmatics tasks such as NEPSY-2 Theory of Mind.
Is caution advised about quick and/or online "Autism Assessments"
We advise caution about quick or on-line Autism "assessments". While rating scales or "screenings" can be helpful in identifying children, adolescents, or adults at risk for Autism Spectrum Disorders, needs for comprehensive pediatric neurological and pediatric neuropsychological assessment of these complex children are critical for diagnostic differential and treatment decisions. Children with ASD often have difficulties staying focused or attending to material they may not be fascinated with, and as with many children in-person face-to-face testing which allows for direct interaction, movement, and physical activity is even more essential than for children in general. Since such a critical diagnosis may follow an individual for much if not all their life, and since this an often-complex disorder, in-person testing is critical to obtain maximal engagement, effort, and validity for anything more than screening.
While rating scales and structured diagnostic interviews are helpful in establishing the diagnosis of ASD, some scales are subject to false positive errors, and these do not provide information about actual neurodevelopmental or neuropsychological deficits.
What is the importance of pediatric neuropsychological assessment of Autism Spectrum Disorders by an experienced Pediatric Neuropsychologist?
Pediatric neuropsychology is a relatively new field with more formal training programs developing in the late 1970's and 1980s. At that time there were very few pediatric neuropsychologists indeed. Dr. Ernest Bordini, Ph.D. trained in neuropsychology at the University of Florida Shands during that period of time and has more than 30 years of practice experience providing in-depth pediatric neuropsychological evaluation of Autism Spectrum Disorder and other childhood neurological, neurodevelopment, and psychiatric disorders. Click for more about his experience as a pediatric neuropsychologist or visit his staff page on this website.
Children, adolescent and adults who suffer from a mild to severe spectrum of disorder can vary quite a bit on some specific areas of functioning including general intelligence, attentional deficits, ability to recognize emotional tone or affect from speech or visual cues, sensory-motor integration, processing and learning styles, expressive and receptive language skills, motor functioning, and executive function skills. Getting the overall picture of this complex disorder by comprehensively assessing the unique needs of a specific child is often critical in guiding educational and treatment planning.
Pediatric neuropsychological assessment or evaluation of such children should address issues of ruling out general developmental delays, assessing language functioning, general intelligence, specific learning disabilities, ruling out co-morbid psychiatric conditions, and assessing nonverbal as well as verbal communications skills. Such evaluation may include special measures to assess ability to recognize emotion in facial expression, tone of voice, and level of interest in reciprocal social interaction. Assessment of sensory-perceptual integration skills, fine and gross motor skills, attention, memory and executive functions will help with differential diagnosis. Comprehensive pediatric neuropsychological assessments of ASD help rule out developmental coordination disorders and sensory-motor integration problems, determine level of disability, levels of needed assistance, guide treatment, need for speech or occupational therapy services, set appropriates expectations, determine needs for accommodations and play an important role in establishment of 504 Plans or Individualized Educational Plans (IEP).
Careful assessment of the relationship between ASD symptoms and neuropsychological functioning is critical for differential diagnosis and treatment planning. Pediatric neuropsychologists have training and experience in the normal developmental stages in cognition, social-perceptual and social-cognitive skills, interpersonal development, language, attention, executive functioning, memory and learning. Pediatric neuropsychological assessments provide an overview of neuropsychological domains as they relate to the evaluation of individuals with Autism Related Disorders.
Issues of severity and general adaptive functioning may play a critical role in diagnostic inclusion with implications for disability determinations, educational determination and accommodations, and individual needs for treatment and therapies. DSM-5 Diagnosis of Autism Spectrum Disorder include specifiers and guidelines with respect to levels of needed functional support. In some cases, forensic neuropsychological evaluations related to legal competencies and needs for guardianship may be required.
How does the Florida Department of Education define Autism Spectrum Disorder?
The Florida Department of Education defines Autism Spectrum Disorder in the following manner: "Autism Spectrum Disorder is defined to be a range of pervasive developmental disorders that adversely affects a student's functioning and results in the need for specially designed instruction and related services. Autism Spectrum Disorder is characterized by an uneven developmental profile and a pattern of qualitative impairments in social interaction, communication, and the presence of restricted repetitive, and/or stereotyped patterns of behavior, interests, or activities. These characteristics may manifest in a variety of combinations and range from mild to severe. Autism Spectrum Disorder may include Autistic Disorder, Pervasive Developmental Disorder Not Otherwise Specified, Asperger’s Disorder, or other related pervasive developmental disorders. The corresponding definition is found in State Board of Education Rule 6A-6.03023, F.A.C."
What are the range of treatments available for Autism Spectrum Disorder?
Early diagnosis of autism spectrum disorder (ASD) coupled with prompt, evidence-based and effective intervention is important for better treatment outcomes. It has been found that early intervention for at least two years before start of school can result in significant improvements, with some being able to enter regular education elementary school settings.
Evidence-based practices for the treatment and management of autism spectrum disorder (ASD) include:
Pivotal Response Training (PRT)
Discrete Trial Teaching
Early Start Denver Model (ESDM),
Antecedent Based Interventions
Differential Reinforcement of Alternative, Incompatible, or Other Behavior Exercise Extinction
Functional Communication Training (FCT)
Parent-Implemented Instruction & Intervention
Picture Exchange Communication System (PECS)
Prompting (including Time Delay) Reinforcement
Response Interruption & Redirection (RIRD)
Self-Management
Visual Supports and Intervention Packages that Utilize EBPs
Lovaas Model
The most effective evidence-based treatments available today are applied behavioral analysis, occupational therapy, speech therapy, physical therapy, and pharmacological therapy.
Assessment helps target treatment to minimize impact of the most pertinent core features and associated deficits of ASD. Pediatric neuropsychological evaluation can often provide specific recommendations for evidence-based areas of intervention for Speech therapy such as interventions for pragmatic communication difficulties, difficulties with verbally labeling emotions in self-and others, nonverbal difficulties, handwriting difficulties or visuospatial difficulties which might require pediatric Occupational therapy (OT), or other neurological or developmental issues which might respond to Physical therapy (PT).
The relative efficacy of autism treatments can vary depending on the individual, their level of functioning and their specific needs. Some interventions are directed at very nonverbal individuals with ASD.
Applied Behavior Analysis has been recognized as an evidence-based practice for ASD, but sometimes has been controversial. Some autism rights activists have expressed concerns with historical events and abuses, raised concerns about aversive procedures, and some ABA goals. Some of the concerns involve the limited emphasis and training in diagnosis, personality, and co-occurring psychiatric conditions involved with application of strict behavioral principals. Distress or regression with treatment may also be a risk.
Pharmacological interventions for may be used to target some of the more severe emotional and behavioral presentations that can be seen, but vary, in children, adolescents, and adults with ASD. Generally, substantial evidence-based supporting medications for ASD is limited. According to an update on psychopharmacological treatments for ADHD, two atypical antipsychotics, risperidone and aripiprazole, have indications for use for severe irritability in children and adolescents with ASD, but these have more serious side-effects than most modern antidepressants. At this time medication use in ASD is considered "off-label" but not uncommon and are often used to treat co-morbid OCD, anxiety disorders, mood disorders, and depression. These may include treatment antidepressants, antipsychotics, anticonvulsants and stimulants. See our discussions on use of antidepressants in teens and pharmacological approaches to treating ADHD for more detailed information about many of these medications and the importance of careful psychological evaluations and follow-up in precenting or avoiding adverse reactions events.
RESOURCES:
Clinical Psychology Associates of North Central Florida offers more than 30 years of experience in conducting complex pediatric neuropsychological assessment of children, adolescents and adults with autism spectrum disorder, ADHD, learning disorders, brain injuries and developmental pediatric neurological disorders. We offer assessments in our Gainesville and Ocala, Florida offices. (352) 336-2888 info@cpancf.com
Additional Resources:
Autism at Yale - Yale University - Evaluation and Research of Autism, Asperger's Syndrome, and the Pervasive Developmental Disorders
References:
Hudson, C.C., Hall, L. & Harkness, K.L. Prevalence of Depressive Disorders in Individuals with Autism Spectrum Disorder: a Meta-Analysis. J Abnorm Child Psychol 47, 165–175 (2019). https://doi.org/10.1007/s10802-018-0402-1
Ketelaars, M. P., Cuperus, J. M., van Daal, J., Jansonius, K., & Verhoeven, L. (2009). Screening for pragmatic language impairment: The potential of the children's communication checklist. Research in Developmental Disabilities, 30(5), 952-960.
All rights reserved:
Clinical Psychology Associates of North Central Florida
Main office: 2121 NW 40th Terrace Suite B, Gainesville, FL 32605
Ocala Satellite Office 3620 NE 8th Place, Ste 3, Ocala, FL 34470
Contact Information: call (352) 336-2888 or email at info@cpancf.com
|
|

